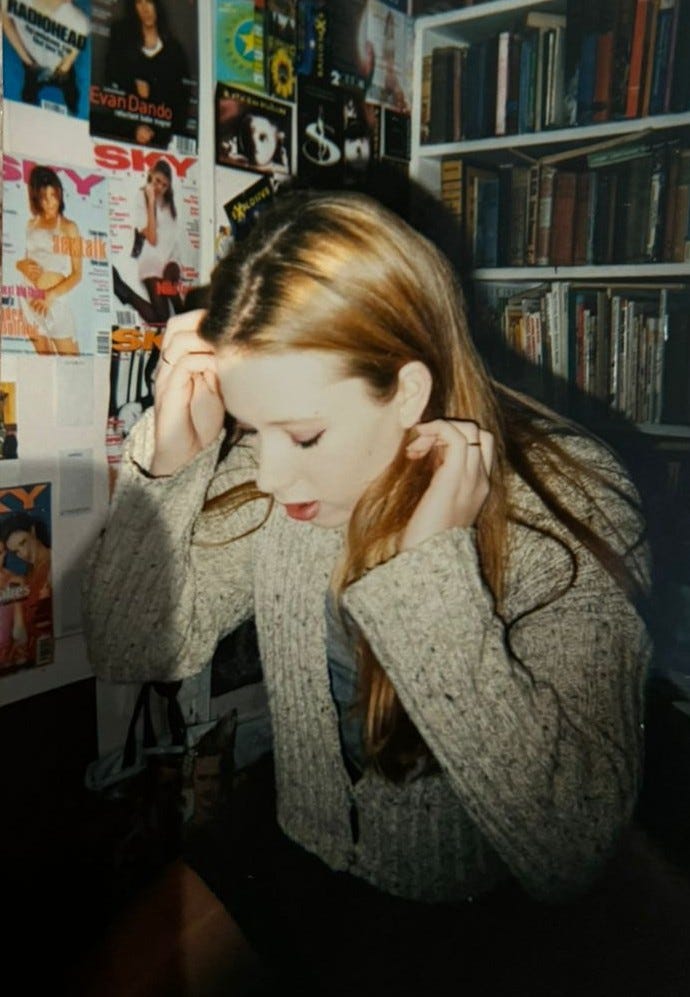
I loved this photo when my oldest friend, Elinor Cleghorn sent it to me from her box of nostalgia, but when I forwarded it onto my daughter, she replied ohhh you look pale.
And I thought about it: yes, I was pale, because I was very unwell. In this photo, (I think taken in 1996) I was probably at my lowest weight, maybe 6.5 stone, roughly 13.9 BMI. I wasn’t trying to lose weight but my throat was so painful I could barely eat. Two years of repeated bouts of tonsillitis and umpteen courses of antibiotics switched on my lurking autoimmune antibodies. 1
Once on, there’s no turning them off.
Something terrible was galvanising at a cellular level. I was hospitalised with gross swelling in the soft tissues of my ankles and knees. Some mornings the doctors brought in colleagues or student medics and they marvelled over my swellings and data, baffled and inquisitive. They didn’t smile at me or make conversation. They talked amongst themselves in a language that made no sense to me because it was technical and full of acronyms. It was as though I’d stepped into an alternative universe, where I had no agency over what happened to me. Student medics peered at my joints. I was a medical marvel, the patient whose symptoms mirrored rheumatic fever, but who tested negative for every known disease that those symptoms align with. I was a teenager with inflammation markers so high they were like an old lady riddled with arthritis.
Had I not been monitored for days in the hospital, the doctors might not have completed all of the tests that meant they found my anti-nuclear antibodies. Autoimmunity isn’t something you can touch or see, unless you know how to look and what test results to screen for; routine blood screenings and even some inflammatory markers won’t show anything untoward. If you have seronegative autoimmunity, the usual markers don’t always show up as raised.
Because I was juvenile and the crisis was so acute, it was given proper attention.
It occurs to me years later that if I had been an adult, this kind of episode might be ignored or I’d have been left to suffer, as many women are, having to endure years of pain before being referred to a specialist. I won’t know it for some time, but I’m lucky it happened like this, and that I was a juvenile, that I wasn’t just another participant in the lost demographic of sick people, whose idiopathic illness remains mysterious for years, if not decades.
For more on misdiagnosis and mystification of women’s bodies, you should read the incredible work, Unwell Women by cultural historian, Elinor Cleghorn. It’s such an important book it has been widely translated and distributed across the world, not least because the issue is so pervasive.
Finally, after investigation, I was diagnosed with an ‘unspecified auto-immune condition’. I learnt enough to know that my antibodies respond to my own cells as though they aren’t part of my body: foreign invaders that need destroying, though I rarely used to give that much detail if somebody asked.
As a teenager, I obsessed over those words ‘disease’, and ‘unspecified.’ So obscure, so evasive. I didn’t have a name for my illness, something I could read about for myself and have people respond, oh, I’ve heard of that. The elusive nature of my disease made it even more complicated to disclose in a simple exchange with a stranger or friend. Back then, I didn’t know anyone else who was chronically sick. It wasn’t that people weren’t sick, there just wasn’t any dialogue happening, there wasn’t the sharing of information, resources, stories, the surge of illness narratives we have now (online) that help us understand ourselves and our bodies. For many many years I didn’t divulge it because I considered my illness to be an ugly part of me, an impairment that I must keep hidden as far as possible. I’ve grown out of that, but let’s call it what it was: internalised ableism.
Instead, if pressed, I used to say my immune system is over-active, which is sort of true, but also reductive. It is more that it misrecognises itself as foreign and attacks itself.
When I came to write about it years later, I realised it would have been useful to have a name for my illness, because there was no nosology or mythology, no medical language to appropriate, play with or shape for poetic purposes.
The unknowability of self:
The mysterious autoimmune processes pose a range of ontological questions to do with the ‘self-non-self’ paradigm of illness. Frederik Svenaeus’ theories of un-home-like-ness and dis-harmonised embodiment are useful, alongside Ed Cohen’s theories of the knotty paradoxes that posits the ‘self’ as a biological organism that is both self and not self, that is, self at war with itself, attempting to destroy itself. 2
The invisible nature of my disease also enabled me to hide it from others.
Autoimmunity is often invisible. Nobody can see my illness. Even on my worst days, no-one would think to look at me and give up their seat for me on public transport. Nobody would know that without medication, I’m too unwell to move, to walk, to wash, to hold a cup, to get dressed. That there have been occasions where I can’t breathe for the pain.
For 20 years, I had hidden my illness, kept it sequestered, but during my PhD, I started to lean toward it. I had been performing the role of a normative body. My disease becoming impossible to ignore, (twenty years of autoimmune destruction resulted in a joint fusion and osteoarthritis, and I had no choice but to take immune-suppression medication I had been terrified of). It was at this point, I decided to make autoimmune illness and representations of the sick body the central focus of my PhD.
At that time, I was thinking a fair amount about the challenges and outcomes arising from interdisciplinary engagement, and the processes and productive tensions created when knowledge and technical information are charged with lyricism. (If you are interested in poetry that sits at the information intersection, and fancy it, you can read an essay I wrote back in 2015 here.) Following this, I started to add the illness experience in, to see what happened when I slipped between the two registers, the technical language of illness and the quotidian experience of being in the world, particularly this performance of wellness.
The idea of the sick body performing invulnerability and wellness became a large preoccupation.
I’m nodding at Joni Mitchell and Susan Sontag, when I say I’ve seen the world from both sides now, because I’ve occupied the kingdom of the sick and the kingdom of the well.
For many years, I was hopeful that if I ignored my illness, if I played it down and didn’t talk about it, it would disappear in much the same way as it had appeared. But it didn’t disappear. If anything it ramped up.
To make my illness the subject of a creative study was also to intellectualise the experience. That has brought with it a whole set of new concerns, and ways of exposing the emotional experience accompanying chronic illness, because the psyche, just as much as the body, also experiences the complexities of that journey. I often think I don’t dwell on the emotional experience enough, and that is something for me to investigate.
At some point, I bought my historic hospital notes for £50, many of which are handwritten.
The clinician’s notes focus on diseases and symptoms that I do not have: The patient denies any history of xxx. This is not xxx disease. This is not xxx syndrome. There was poetry in the repetition of what I do not have. This became the basis of a collaborative poem title ‘with sequelae’ between myself and Elinor Cleghorn (we start three minutes in). Our intention was to examine the tensions between the clinical language of objective science and the subjective realm of lived experience. At first, the poem was quite technical with us both using our medical notes, and we deliberately sought ways to lighten the tone. We appropriated lyrics, reported speech from our respective children and parents, and placed these alongside well-minded but absurd suggestions that friends, acquaintances and strangers offer on coping with acute periods of illness, as if we hadn’t tried everything possible. These iterations begin ‘have you tried… [insert a miracle cure]?’ Some of these absurd suggestions are included verbatim, others are satirised to the point of ridiculous. The point is, no yoga class or medicines you can buy over the counter can cure autoimmunity.
Just this week, I said the words ‘have you tried honey?’ to a friend with a pollen allergy and was reminded of mine and Elinor’s poem again. Recently, I found myself saying ‘have you tried listening to pineal gland videos on YouTube’ to a friend with insomnia. Well, OF COURSE she had tried that, she probably knows more about insomnia than most sleep clinic doctors, let alone me, who has only suffered with sleep issues during acute life crises. And haven’t I found myself knowing more about autoimmunity than the majority of general practitioners. We recognise how it waxes and wanes, hiding and then flaring up with unstoppable force. We implicitly know the difference between growing pains and injury, and sudden, acute, reactive or rheumatic autoimmune swelling.
But let’s keep in mind that it is always well-minded advice. We can’t help but want to help each other because we have spent years, (often decades) looking for solutions that might alleviate our symptoms and suffering even a tiny bit. For me, curiously, I found avoiding the nightshade and rutaceae group of foods helped. It did not cure or wipe out flares completely but I had discovered I was specifically reactive to those families. I endured many years of pain and suffering before giving in and taking the hard-core disease modifiers, which I’ll admit, have been life changing.
That sixteen-year-old in the picture above had no idea how that autoimmune illness would change her life so dramatically. My relationship to her is fairly complicated, for many reasons. One of them is the belief I once held — that disability and illness were caused by sinful activities, possession, evil spirits, or dabbling with the occult. For many years, I believed my illness was a punishment for wild and shameful behaviour. My childhood was seeded with ceremony, incantatory prayer, sacred words, Latin song, hymns, and chanting. I was taken on religious pilgrimages, provoking a fascination for sites where Catholics continue to pilgrim for treatment, purification, and remedy. This so-called 'truth' was a constructed framework. It was another form of internalised ableism, woven into the fabric of the religious culture I was raised within.
Chronic illness may have taken so much from me, but it also shaped me and has given me purpose, meaning, a community. The sick community write for each other, to help each other understand the philosophical complexities and resonances of chronic illness, disease and sequelae. We are hungry for each others’ stories, for solidarity and understanding.
I’m hoping to post soon write about this wonderful and groundbreaking inquiry, Dreaming in the Fault Zone: a poetics of healing by Eleni Stecopoulos and am excited to follow up that post with a write up of Khairani Barokka’s nonfiction debut, Annah, Infinite.
Watch this space.
There are theories about epigenetics, environment, oral-gut translocations, toxin biomarkers, microbiomes and parasites, but perhaps that’s for another post.
Svenaeus, F. (2000). The body uncanny--further steps towards a phenomenology of illness. Medicine Health Care and Philosophy. 3(2)There are theories about epigenetics, environment, oral-gut translocations, biomarkers, parasites, but perhaps that’s for another chat., 125-37.
Svenaeus, F. (2010). Illness as unhomelike being-in-the-world: Heidegger and the phenomenology of medicine. Medicine Health Care and Philosophy. 14(3), 333-343.